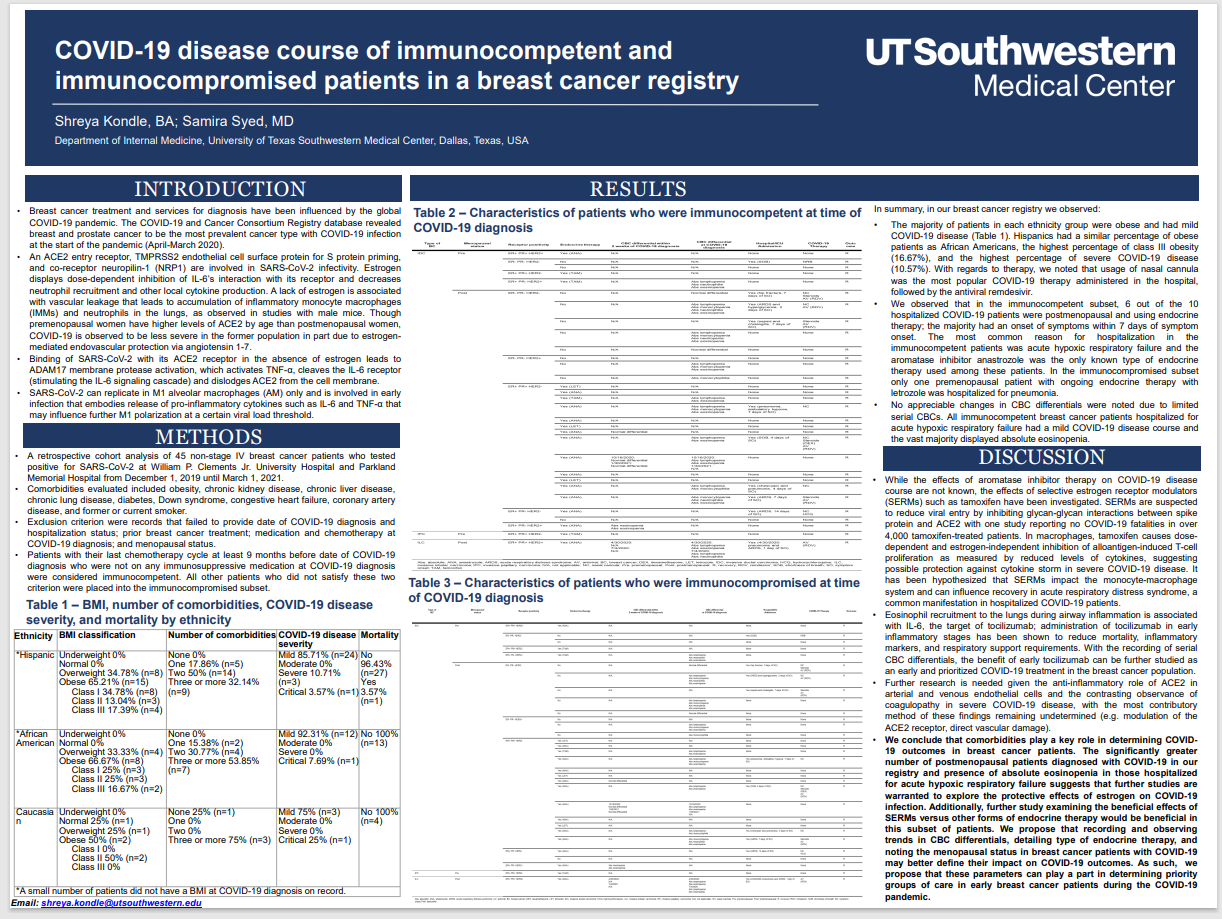
Poster: COVID-19 Disease Course of Immunocompetent and Immunocompromised Patients in a Breast Cancer Registry
Authors: Shreya Kondle, BA; Samira Syed, MD
The COVID-19 pandemic has impacted nearly ever aspect of healthcare, including breast cancer diagnosis and treatment. As a result, researchers with the Department of Internal Medicine at the University of Texas Southwestern Medical Center in Dallas wished to study the course of COVID-19 disease in immunocompetent breast cancer patients versus those who were immunocompromised.
To understand the researchers’ work, it’s essential to understand this background:
- An ACE2 entry receptor, TMPRSS2 endothelial cell surface protein for S protein priming, and co-receptor neuropilin-1 (NRP1) are involved in SARS-CoV-2 infectivity. Estrogen displays dose-dependent inhibition of IL-6’s interaction with its receptor and decreases neutrophil recruitment and other local cytokine production. A lack of estrogen is associated with vascular leakage that leads to accumulation of inflammatory monocyte macrophages (IMMs) and neutrophils in the lungs. Although premenopausal women have higher levels of ACE2 than postmenopausal women, COVID-19 has been observed to be less severe in the former, in part due to estrogen-mediated endovascular protection via angiotensin 1-7.
- Binding of SARS-CoV-2 with its ACE2 receptor in the absence of estrogen leads to ADAM17 membrane protease activation, which activates TNF-a, cleaves the IL-6 receptor (stimulating the IL-6 signaling cascade), and dislodges ACE2 from the cell membrane.
- SARS-CoV-2 can replicate in M1 alveolar macrophages (AM) only and is involved in early infection that embodies release of pro-inflammatory cytokines such as IL-6 and TNF-a that may influence further M1 polarization at a certain viral load threshold.
The researchers’ approach to their question was a retrospective cohort analysis of 45 non-stage IV breast cancer patients who tested positive for SARS-CoV-2 at two hospitals from December 1, 2019 to March 1, 2021. Patients who completed their last chemotherapy cycle at least 9 months prior to the date of their COVID-19 diagnosis and were not on immunosuppressive medication at diagnosis were classified as immunocompetent. Patients who did not meet these criteria were placed in the immunocompromised subset.
The researchers observed that in the immunocompetent subset, 6 of 10 hospitalized COVID-19 patients were postmenopausal and using endocrine therapy. The most common reason for hospitalization in these patients was acute hypoxic respiratory failure. The aromatase inhibitor anastrozole was the only known endocrine therapy in use in these patients.
In the immunocompromised subset of patients, only one premenopausal patient with ongoing endocrine therapy was hospitalized for pneumonia.
All immunocompetent patients hospitalized for acute hypoxic respiratory failure had a mild COVID-19 disease course. The majority displayed absolute eosinopenia.
In their discussion, the researchers concluded that the significantly greater number of postmenopausal patients in the registry diagnosed with COVID-19 and the presence of absolute eosinopenia in those hospitalized for acute hypoxic respiratory failure “suggests that further studies are warranted to explore the protective effects of estrogen on COVID-19 infection.” They also stated that noting the menopausal status of breast cancer patients with COVID-19 could impact treatment and outcomes.