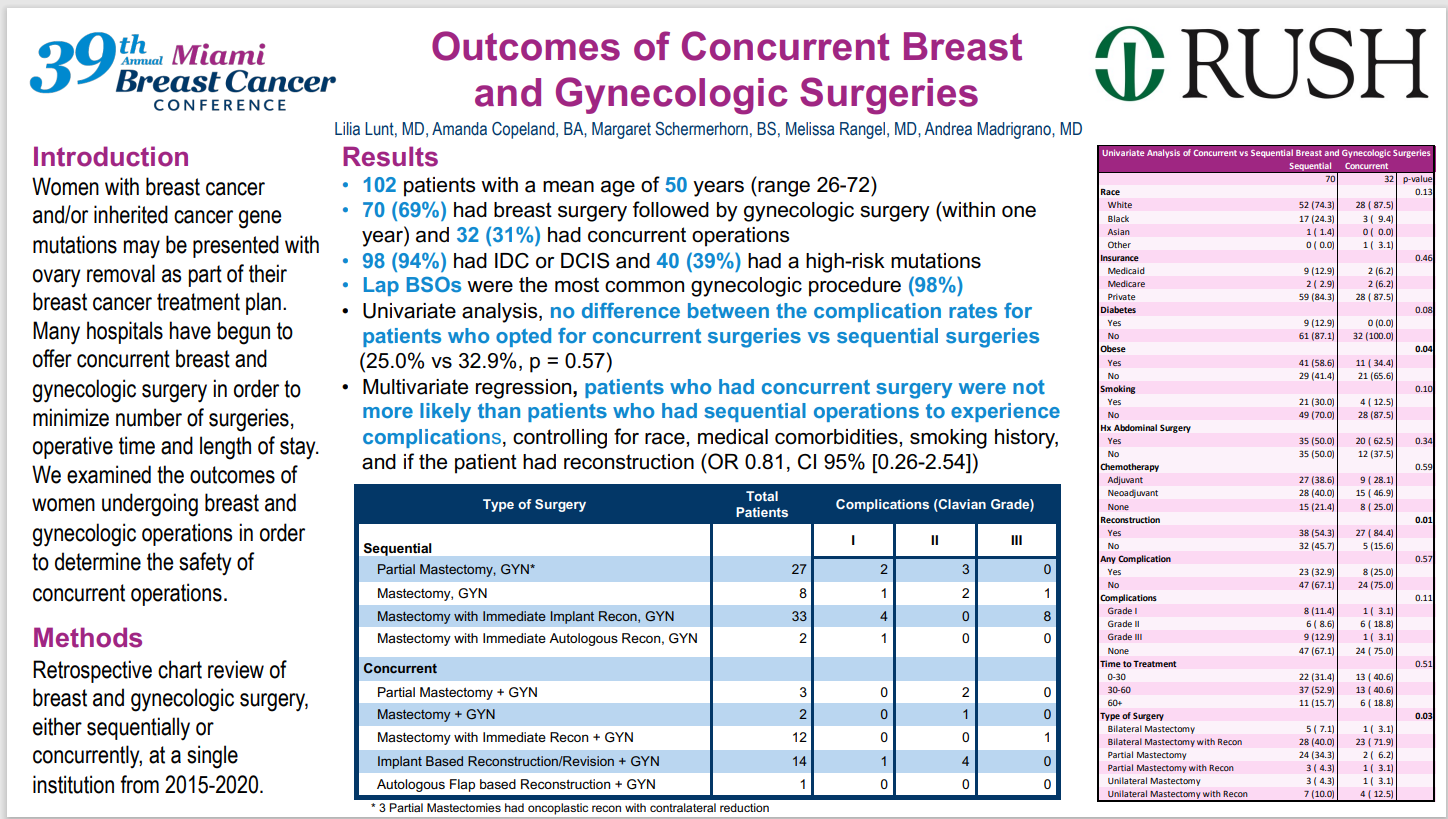
Poster: Outcomes of Concurrent Breast and Gynecologic Surgeries
Authors: Lilia Lunt, MD; Amanda Copeland, BA; Margaret Schermerhorn, BS; Melissa Rangel, MD; Andrea Madrigrano, MD
Women with breast cancer and/or inherited cancer gene mutations are often offered ovary removal as part of their breast cancer treatment. As a result of this, many hospitals have begun to offer these patients concurrent breast and gynecologic surgery in order to minimize the number of surgeries for patients. The approach also minimizes the patients operative time and length of hospital stay.
The poster authors wished to examine the outcomes for women undergoing breast and gynecologic operations in an effort to determine the safety of concurrent operations.
The researchers’ approach focused on a retrospective review of the charts of patients undergoing breast and gynecologic surgery, either sequentially or concurrently, at Rush University Medical Center, Chicago, from 2015 to 2020.
The researchers’ review encompassed 102 patients with a mean age of 50 years. Seventy, or 69%, had breast surgery followed within one year by gynecologic surgery. Approximately one third, 32, had concurrent surgeries. Almost all patients (98/94%) had invasive ductal carcinoma (IDC) or ductal carcinoma in situ (DCIS). Forty (39%) were found to have a high-risk mutation.
Univariate analysis showed no difference between the complication rates for patients who opted for concurrent surgeries versus those who opted for sequential surgeries (25.0% vs 32.9%, p =0.57). Multivariate regression also showed no difference in the likelihood of complications for patients who had concurrent surgery versus those who had sequential surgery, after controlling for race, comorbidities, smoking history, and whether or not the patient had reconstruction (OR 0.81, CI 95% [0.26-2.54].
In summary, the results showed no reason for patients or healthcare providers to avoid concurrent breast and gynecologic surgeries in women with breast cancer and/or inherited gene mutations.